Agentic AI in Claims: Stop Automating Broken Processes
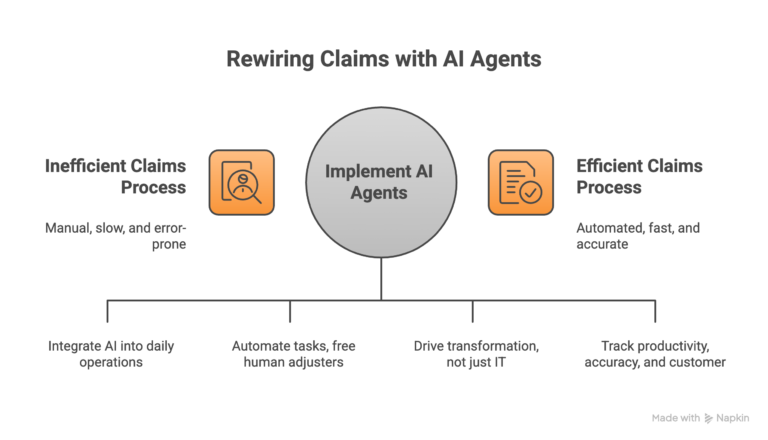
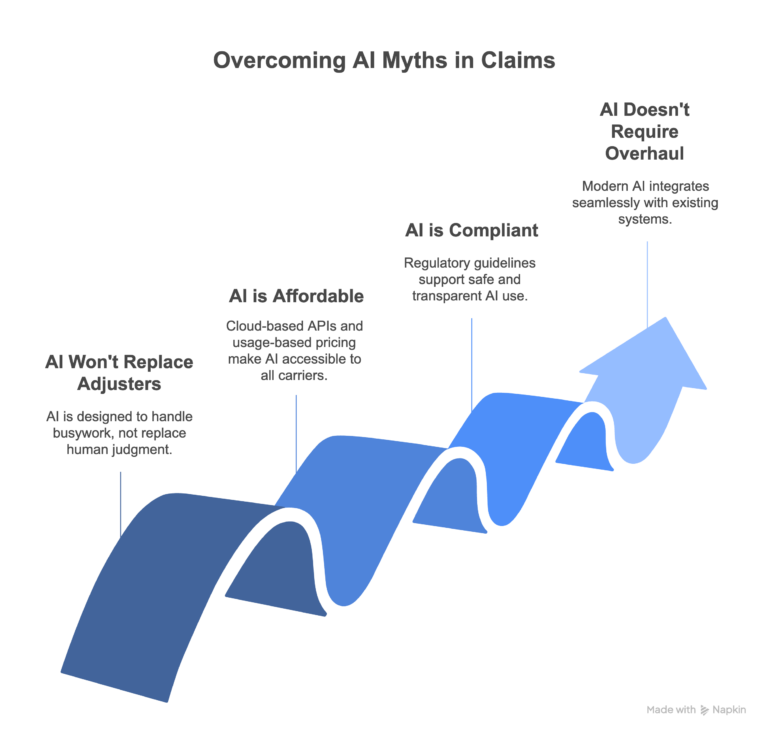
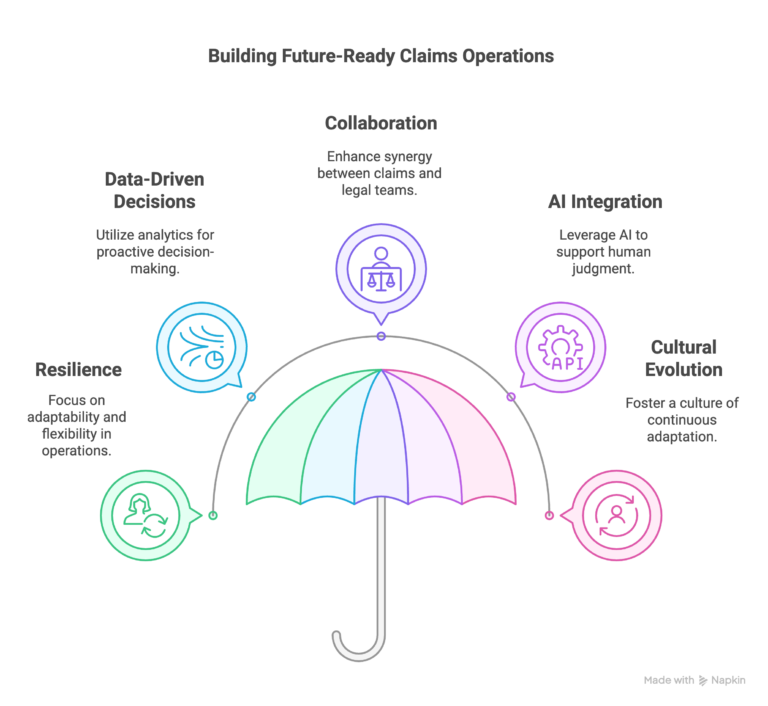
Most claims teams bolt AI onto workflows that were broken before the technology arrived. Here’s what actually works, and what I learned building it. A few years ago, I got tired of watching the same audit cycle play out: weeks of file selection arguments, inconsistent reviewer standards, and findings that arrived too late to change…