Most claims teams bolt AI onto workflows that were broken before the technology arrived. Here’s what actually works, and what I learned building it.
A few years ago, I got tired of watching the same audit cycle play out: weeks of file selection arguments, inconsistent reviewer standards, and findings that arrived too late to change anything. So I built The Audit Portal.
The idea was simple. Use AI to select the right claim files for assessment, standardize how reviewers evaluate them, and automate the analysis. What used to take weeks collapsed into days. More importantly, it created something claims leaders rarely get: an instant feedback loop they could actually trust and act on [1].
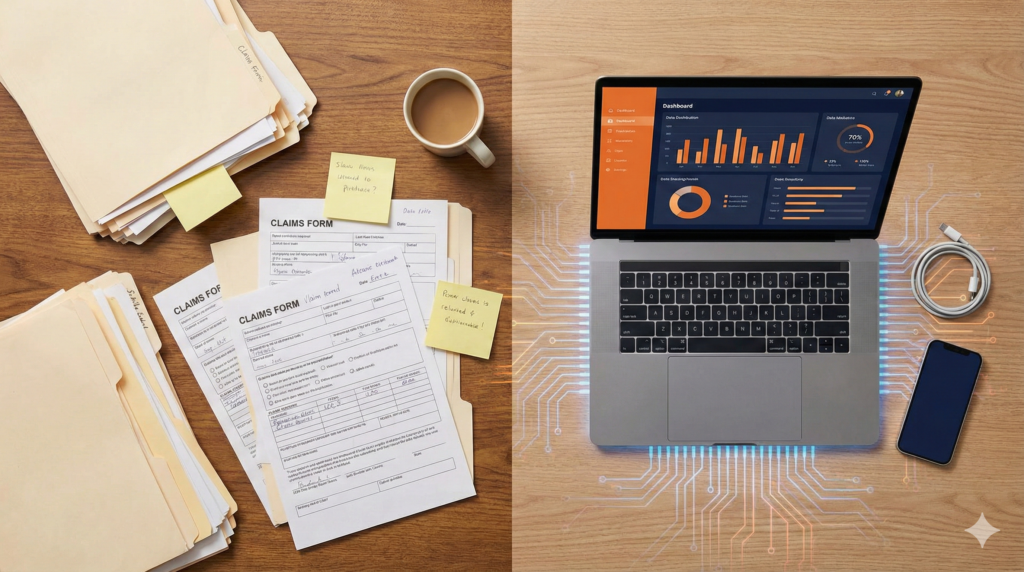
That project confirmed something I’d suspected for years: the problem in most claims operations isn’t a lack of technology. It’s that the underlying processes are broken, and we keep layering tools on top of them.
The Numbers Are Worse Than You Think
If you run a claims operation, you already know this intuitively. But the data makes it hard to ignore:
- 71 to 90% of claims operations still rely on manual processing [2]. That’s not a technology gap. It’s an operating model stuck in the past.
- Claims handling eats 55 to 75% of operational costs depending on the line [3]. And most of that cost is people doing repetitive work that doesn’t require human judgment.
- 11% of settlements are mismanaged due to errors and workflow inefficiencies [4]. Not because adjusters are bad at their jobs, but because the systems they work in set them up to fail.
- Manual claims cost $2.05 to $10.00 per claim more than automated equivalents [5]. Multiply that across your volume and the waste is staggering.
Less than 10% of carriers have achieved full automation in claims processing [6]. That’s a massive gap between what’s possible and what’s actually happening.
Why Smart Organizations Stay Stuck
I’ve consulted with enough claims teams to know the barriers aren’t usually technical. They’re organizational.
Legacy infrastructure is real, but it’s also the excuse that kills more modernization projects than any actual system limitation. I’ve seen teams running 15-year-old platforms who found ways to deploy targeted AI solutions in weeks, simply because someone decided the status quo was no longer acceptable.
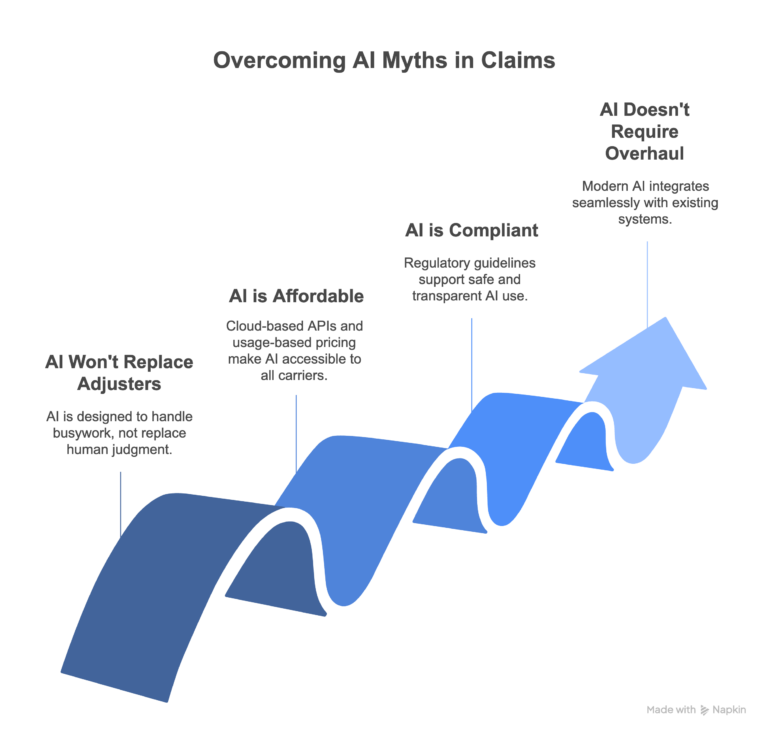
Change resistance runs deeper than people admit. When I talk to claims leaders about agentic AI, the pushback rarely sounds like “we don’t believe in AI.” It sounds like “Our adjusters won’t use it” or “IT won’t approve it.” Both are solvable, but only if leadership treats them as implementation problems, not reasons to wait.
The gains get underestimated. Document processing accuracy improvements of 70%, significant reductions in error rates, and dramatic drops in cycle time [7]. These aren’t theoretical. They’re happening at organizations that committed to rethinking workflows, not just buying software.
What Actually Works: Four Moves That Matter
Based on what I’ve seen work, both at Lanzko and in the claims operations I’ve led, here’s where agentic AI delivers real value:
1. Automate the intake, not the judgment. Routine claims (low-severity, clear-cut liability, standard coverage) don’t need a human to open a file, key in data, and assign it. Agentic AI can handle initial triage, data extraction, and routing so adjusters start their day working cases that actually need them. The goal isn’t to remove people. It’s to stop wasting their time on tasks a machine handles better.
2. Use predictive analytics to prioritize, not just predict. Every carrier talks about predictive models. The ones that get real value use them operationally, flagging high-severity claims at first notice so they get senior examiner attention from day one, not after three months of drift. Early intervention on complex claims is where the real savings hide.
3. Build multi-agent systems for end-to-end workflows. This is where agentic AI earns its name. Instead of one tool doing one task, you design systems where multiple AI agents collaborate across the lifecycle. One handles document classification, another manages coverage verification, a third monitors for litigation triggers. They work together the way a well-run claims team does, except they don’t take lunch breaks or miss diary dates.
4. Deploy document intelligence where it hurts most. Every claims team I’ve worked with loses hours to manual data extraction: pulling information from medical records, police reports, counsel status letters, and invoices. AI-powered document intelligence doesn’t just read faster; it classifies, cross-references, and flags inconsistencies that human reviewers miss under volume pressure.
What This Looks Like in Practice
A major U.S. travel insurance company was drowning in manual processing. Claims took weeks. Adjusters spent more time on data entry than decision-making. After implementing an agentic AI framework across their claims workflow, they automated 57% of their claims processes, reducing processing times from weeks to minutes [8].
That’s not a pilot. That’s a fundamental redesign of how claims work gets done. And it’s the kind of result I see when organizations commit to rethinking the workflow itself, not just bolting automation onto a broken process.
A Word on Governance
I’m bullish on agentic AI in claims, but I’m equally insistent on governance. Any AI system making decisions that affect policyholders needs to be explainable. Not just to regulators, but to the claims leaders accountable for those outcomes [9].
That means transparent decision rationale, human oversight on high-stakes determinations, and audit trails that can withstand scrutiny. If you can’t explain why the AI made a recommendation, you shouldn’t be acting on it. Speed without accountability isn’t efficiency. It’s risk.
The Real Question
The question isn’t whether AI will transform claims operations. It will. The question is whether your organization will lead that transformation or react to it.
From my experience, the claims teams that get the most out of agentic AI share three traits: leadership that owns the change (not IT), a willingness to redesign workflows before deploying technology, and clear metrics for what success looks like. Everything else is implementation.
If your claims operation is exploring how to integrate agentic AI, or trying to figure out why a previous attempt didn’t deliver, I’d welcome the conversation. Reach me at mlanzkowsky@lanzko.com or visit lanzko.com.
Sources
[1] Based on Lanzko Audit Portal implementation outcomes. Details available at lanzko.com/audit-portal.
[2] Accenture, “Technology Vision for Insurance 2024,” reporting 71 to 90% of claims operations reliant on manual processing.
[3] McKinsey & Company, “The Future of AI in the Insurance Industry,” 2024. Claims handling costs represent 75% of operational costs in motor insurance and 55% in home insurance.
[4] Deloitte, “Insurance Claims Management: Navigating the Digital Shift,” 2024. 11% of settlements mismanaged due to errors and workflow inefficiencies.
[5] Capgemini, “World Insurance Report 2024.” Manual claims processing costs $2.05 to $10.00 per claim more than automated processing.
[6] Accenture, “Technology Vision for Insurance 2024.” Less than 10% of insurers achieve full automation in claims processing.
[7] ScienceSoft, “Artificial Intelligence for Insurance Claims in 2025,” reporting 70% improvement in document processing accuracy and significant error rate reductions.
[8] InsurTech case study reported by Oliver Wyman, “Digital Transformation in Travel Insurance,” 2024. Major U.S. travel insurer automated 57% of claims processes.
[9] NAIC Model Bulletin on the Use of Artificial Intelligence Systems by Insurers (2024). As of March 2025, 24 U.S. states have adopted AI governance requirements for insurers.ome the conversation. Reach me at mlanzkowsky@lanzko.com or visit lanzko.com.